Image credit: Laura Liedo for Parents
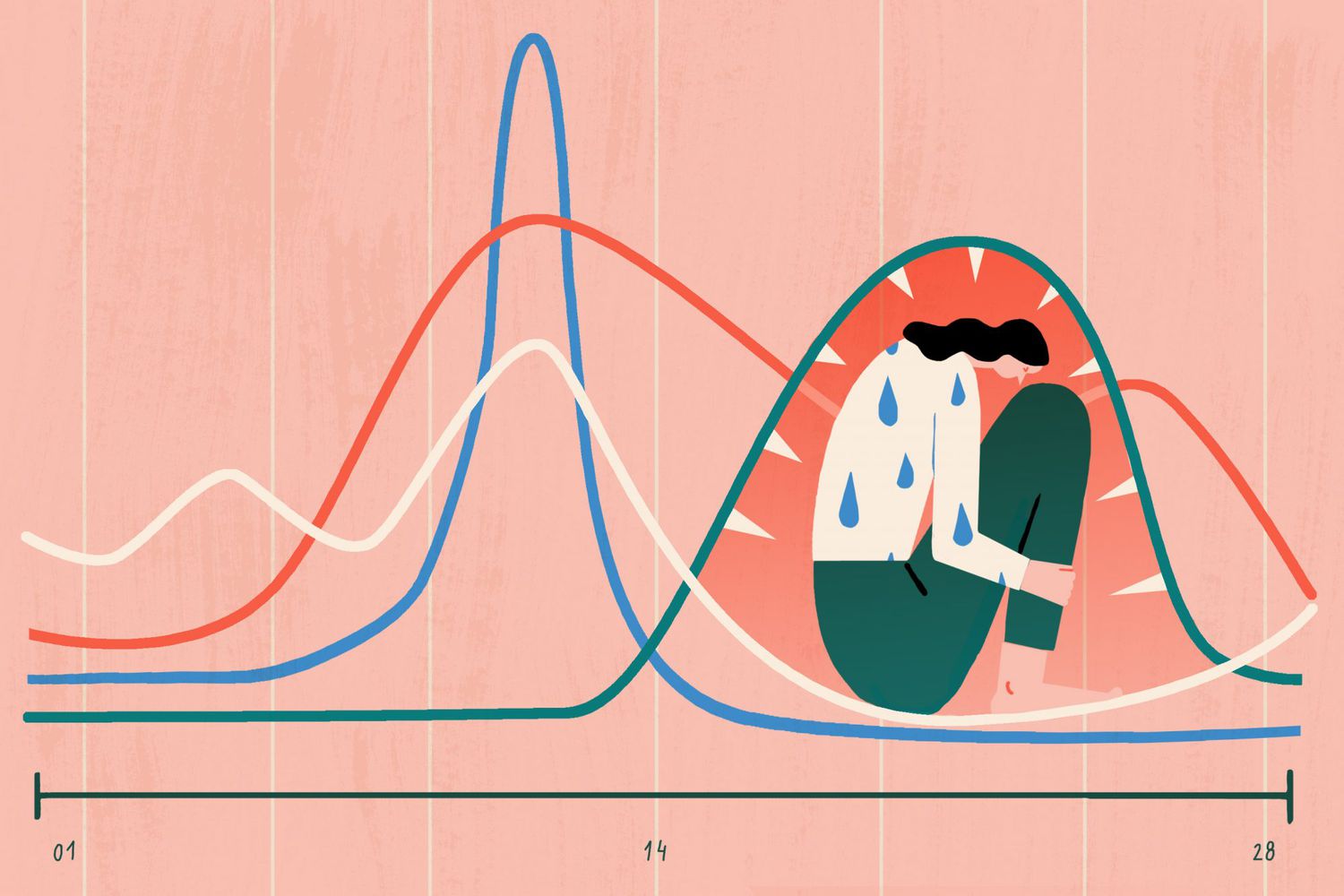
Premenstrual dysphoric disorder (PMDD) is a severe case of premenstrual syndrome (PMS), which affects women both physically and psychologically. A study by Schoep et al. that was conducted in 2019 on more than 30,000 women in the Netherlands, found that 81% of them reported reduced work productivity due to menstruation-related symptoms for an average of 23 days per year. With such a huge impact, it is surprising how little PMDD is talked about. As with many (mental) health issues, the severity of PMDD falls on a spectrum. From no symptoms at all to the most severe forms of PMDD, almost all women are affected at some point in their lives. While clinically diagnosable PMDD is estimated to affect approximately 1.8 to 5.8% of women (American Psychiatric Association, 2013), as many as 18% of women are believed to suffer with subclinical or subthreshold PMDD (Wittchen, Becker, Lieb, & Krause, 2002).
So what exactly is PMDD and how is it diagnosed?
A crucial aspect of PMDD is the timing of symptoms. In PMDD, symptoms must be present in the majority of menstrual cycles that occurred in the preceding year. At least five of the following diagnostic criteria must be present in the final week before the onset of menstruation, start to improve within a few days after the onset of menstruation, and become minimal or absent in the week post-menstruation (American Psychiatric Association, 2013). This distinguishes PMDD from other mental health disorders, which may present in a similar way e.g. depressive or anxiety disorders, which present consistently, while PMDD presents cyclically.
Diagnostic criteria
- Affect lability (e.g. mood swings; feeling suddenly sad or tearful, or increased sensitivity to rejection).
- Irritability or anger or increased interpersonal conflicts.
- Depressed mood, feelings of hopelessness, or self-deprecating thoughts.
- Anxiety, tension, and/or feelings of being keyed up or on edge.
- Decreased interest in usual activities (e.g., work, school, friends, hobbies).
- Subjective difficulty in concentration.
- Lethargy, fatigue, or marked lack of energy.
- Change in appetite; overeating; or specific food cravings.
- Hypersomnia or insomnia.
- A sense of being overwhelmed or out of control.
- Physical symptoms such as breast tenderness or swelling, joint or muscle pain, a sensation of “bloating”, or weight gain.
- Finally, symptoms are associated with clinically significant distress or interference with work, school, usual social activities, or relationships with others (e.g. avoidance of social activities; decreased productivity and efficiency at work, school, or home).
What causes PMDD?
While the cause of PMDD is not yet completely understood, it is hypothesized that a number of variables (see below) are responsible for the development and maintenance of PMDD symptoms (American Psychiatric Association, 2013).
- Hormonal imbalances and/or severe reactions to normal hormonal fluctuations (namely progesterone, estrogen)
- Stress
- History of interpersonal trauma
- Seasonal changes e.g. seasonal affective depression (SAD)
- Sociocultural aspects of female sexual behaviors and female gender role
- Genetic factors (heritability is unknown, but estimates range from 30% to 80%)
Myths and misdiagnoses
Myth #1: PMDD is normal, it’s just part of being a women
Social and cultural stigma still surrounds issues related to menstruation. Many women minimize the seriousness of their complaints, and can also be dismissed by healthcare professionals who are not familiar with PMDD.
Myth #2: PMDD is the same as PMS
PMS is not the same as PMDD. PMS is a colloquial term, not a clinical diagnosis. If anything, PMS is a less severe form of PMDD.
Misdiagnosis #1: dysmenorrhea (period cramps or heavy periods)
Dysmenorrhea is a syndrome of painful menses, but distinct from PMDD as it does not include affective (mood) changes. Symptoms of dysmenorrhea begin at the onset of the bleeding, whereas symptoms of PMDD are present before the onset of bleeding.
Misdiagnosis #2: bipolar disorder
Bipolar disorder consists of depressive episodes and (hypo)manic episodes, but generally does not follow the menstrual cycle.
CBT as a treatment for PMDD
Cognitive behavioral therapy (CBT) is a therapeutic approach with a strong evidence-base to support it. In CBT therapy, the focus is placed on the connection between your thoughts, emotions and behaviors. Clients in CBT therapy identify the negative or unhelpful patterns they engage in, and learn to change these into more realistic and helpful ones. Through actively engaging in therapy, clients gain insights into the potential reasons that led to the development and maintenance of their symptoms, as well as their individual triggers and responses. As a structured and practical therapeutic style, CBT also teaches individuals easy and applicable tools and coping strategies.
- Guided discovery helps individuals to see evidence for and against their beliefs and assumptions, and challenges them to broaden their perspective.
- Cognitive restructuring helps to identify negative and biased thought patterns and reframes them.
- Exposure therapy can be used to confront feared situations, for example social situations that induce anxiety.
- Habit building aims to create lasting healthy habits.
- Activity scheduling and behavioral activation encourage the incorporation of positive activities into day-to-day life, and help with the reduction of activity avoidance (e.g. due to anxiety or procrastination).
- Core beliefs about the self, others, and the world are examined in CBT. This can include societal norms, beliefs, attitudes, and stereotypes regarding gender and the menstrual cycle.
- Emotion regulation skills can help individuals in managing strong emotions like anger, fear, sadness, and grief.
- Relaxation and stress reduction techniques like deep breathing exercises, muscle relaxation, and imagery are also often used in CBT.
Evidence for the use of CBT for PMDD
- In one randomized comparison study, CBT was shown to be an effective treatment for PMDD and was associated with better maintenance of treatment effects 1 year post-treatment compared with antidepressant fluoxetine (Hunter et al., 2002).
- In a randomized controlled trial (RCT), online CBT therapy was shown to be highly effective in reducing PMDD symptoms by addressing coping styles and stress management in treatment (Weise et al., 2019).
- Interestingly, a systematic literature review found that in all 32 studies identified, there was a significant reduction in PMDD symptoms (in some even a total remission). Interestingly, online-delivered self-help tools were good enough for most women to manage their PMS distress, with only the most severe PMS forms requiring one-to-one CBT (Kancheva Landolt & Ivanov, 2021).
Holistic treatments
Due to the interplay of biological and psychological factors present in PMDD, it’s crucial to adopt a comprehensive treatment approach that addresses both physical and mental aspects. A holistic approach to treatment considers an individual’s lifestyle factors like diet, sleep, exercise, relationships, and sources of stress. Nutrition and exercise can positively impact mood and energy levels, and building support networks can help in providing a sense of community and understanding. Since PMDD affects so many facets of life, it is important to take a big picture approach to its treatment. Several other practices like journaling and mindfulness can complement the journey to managing PMDD. Journaling can allow individuals to better keep track of emotional fluctuations, identify recurring themes in symptoms, and organize their thoughts. Mindfulness practices can help decrease stress and anxiety. These options are also great starting points in case therapy is not an option.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders(5th ed.). doi.org/10.1176/appi.books.9780890425596
Hunter, M. S., Ussher, J. M., Browne, S. J., Cariss, M., Jelley, R., & Katz, M. (2002). A randomized comparison of psychological (cognitive behavior therapy), medical (fluoxetine) and combined treatment for women with premenstrual dysphoric disorder. Journal of Psychosomatic Obstetrics & Gynecology, 23(3), 193-199. doi.org/10.3109/01674820209074672
Kancheva Landolt, N., & Ivanov, K. (2021). cognitive behavioral therapy-a primary mode for premenstrual syndrome management: systematic literature review. Psychology, Health & Medicine, 26(10), 1282-1293. doi.org/10.1080/13548506.2020.1810718
Schoep, M. E., Adang, E. M., Maas, J. W., De Bie, B., Aarts, J. W., & Nieboer, T. E. (2019). Productivity loss due to menstruation-related symptoms: a nationwide cross-sectional survey among 32 748 women. BMJ open, 9(6). doi:10.1136/ bmjopen-2018-026186
Weise, C., Kaiser, G., Janda, C., Kues, J. N., Andersson, G., Strahler, J., & Kleinstäuber, M. (2019). Internet-based cognitive-behavioral intervention for women with premenstrual dysphoric disorder: a randomized controlled trial. Psychotherapy and psychosomatics, 88(1), 16-29. doi.org/10.1159/000496237
Wittchen, H. U., Becker, E., Lieb, R., & Krause, P. (2002). Prevalence, incidence and stability of premenstrual dysphoric disorder in the community. Psychological medicine, 32(1), 119-132. doi.org/10.1017/S0033291701004925
Advantages of Discovering Your Therapist via It’s Complicated
- No Setup Costs: Creating an account and reaching out to therapists is entirely cost-free.
- Transparent Pricing: You’ll only pay the session fee, with no concealed booking fees.
- Precise Search: Utilise our robust search tool to pinpoint therapists based on your specific preferences.
- Thorough Listings: Easily explore therapists categorised by their specialty, approach, location, and language.
It’s Complicated is a therapy platform that not only helps clients find their perfect therapist but also supports therapists in their craft of helping others. Featuring over 2,000 mental health professionals from 80+ countries, counselling is available in almost 100 languages, both online and in person. A GDPR-compliant video solution, encrypted messaging, and easy invoicing guarantee a private and seamless counselling experience for therapists and clients alike. If you are in a serious crisis and need urgent help, please use one of these resources instead.